Kennedy ulcers, also known as Kennedy terminal ulcers, are a type of skin lesion that can appear on the skin of individuals, particularly the elderly, who are nearing the end of their life. These ulcers are often seen as a sign of the body's natural decline and can be a challenge to manage. Understanding what Kennedy ulcers look like can help in their identification and treatment. Below are descriptions and discussions related to Kennedy ulcers, keeping in mind the importance of professional medical diagnosis and care.
Understanding Kennedy Ulcers

Kennedy ulcers are typically characterized by their shape, size, and location on the body. They can appear as oval or circular patches on the skin, often with a distinct edge. The size can vary, but they are usually several centimeters in diameter. These ulcers can develop on various parts of the body, including the buttocks, hips, and lower back, areas that are under pressure when a person is bedridden or has limited mobility.
Visual Identification
Visual identification of Kennedy ulcers involves looking for areas of the skin that are red, purple, or black, which can indicate tissue damage due to poor blood circulation. The skin around the ulcer may be swollen and feel warm to the touch. In some cases, the ulcer may break down further, leading to open sores that can be painful and prone to infection. It’s crucial to approach any skin lesion with caution and seek medical advice to ensure proper diagnosis and treatment.
| Characteristics | Description |
|---|---|
| Shape | Oval or circular |
| Size | Several centimeters in diameter |
| Location | Buttocks, hips, lower back |
| Color | Red, purple, or black |
| Surrounding Skin | Swollen, warm to the touch |

Key Points
- Kennedy ulcers are skin lesions that can appear in the elderly or those nearing the end of life.
- They are often found on areas under pressure, such as the buttocks and lower back.
- Visual identification involves looking for red, purple, or black patches on the skin.
- Seeking medical advice is crucial for proper diagnosis and treatment.
- Early care and management can improve the quality of life for affected individuals.
Managing and Treating Kennedy Ulcers
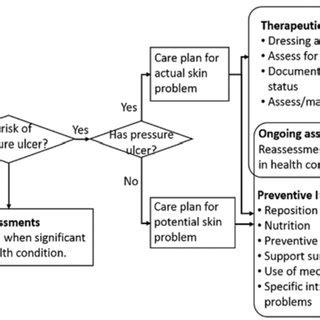
Managing Kennedy ulcers involves a comprehensive approach that includes relieving pressure on the affected areas, improving circulation, and preventing infection. This can involve repositioning the individual regularly, using support surfaces designed to reduce pressure, and keeping the ulcer clean and dry. In some cases, medical treatments such as debridement (removing dead tissue) or the application of topical treatments may be necessary.
Prevention Strategies
Preventing Kennedy ulcers from developing in the first place is a key aspect of care. This can involve regular skin inspections, especially in areas prone to pressure sores, ensuring good nutrition and hydration to support skin health, and encouraging mobility and activity as much as possible. For individuals who are bedridden, using devices that can help reduce pressure, such as air mattresses or foam wedges, can be beneficial.
Understanding and addressing Kennedy ulcers requires a compassionate and informed approach. By recognizing the signs and taking proactive steps towards prevention and treatment, we can improve the comfort and dignity of individuals in their final stages of life.
What are Kennedy ulcers, and how do they appear?
+Kennedy ulcers are skin lesions that can appear on individuals nearing the end of life, particularly on areas under pressure like the buttocks and lower back. They are characterized by their oval or circular shape and can be red, purple, or black in color.
How are Kennedy ulcers managed and treated?
+Management involves relieving pressure, improving circulation, and preventing infection. This can include repositioning, using support surfaces, keeping the area clean, and in some cases, medical treatments like debridement or topical applications.
Can Kennedy ulcers be prevented?
+Prevention strategies include regular skin inspections, ensuring good nutrition and hydration, encouraging mobility, and using devices that reduce pressure on vulnerable areas. Early detection and intervention can significantly improve outcomes.